Danisha Christian and Rahul Gupta contributed to this series
“In the last ten years alone, there have been instances of medical neglect, sexual abuse, and preventable suicide in private facilities [throughout the state], said Bob Libal, Director of Grassroots Leadership. Libal and others are part of the Texas Civil Rights Project and Prison Legal News lawsuit against Corrections Corporation of America. CCA is one of the top two private prison companies in the country.
Private prisons throughout the country have faced charges from family members and advocates, alleging the wrongful death of inmates whose medical conditions were not only treatable, but routine and preventable. While many of the cases included in this article point to the state of Texas—that state is not an outlier, but part of the norm.
In the realm of healthcare reform discussions, prison populations and medical care rarely spark the attention they deserve. The United States has the highest incarceration rate in the world with 1 out of every 100 people in America is behind bars; with 1 in 3 African American males coming in contact with the prison system. We devote $74 billion to our prisons annually, and yet the majority of inmates lack access to many of the most basic health care services.
“The number of inmates in private prisons increased by roughly 1600 percent between 1990 and 2009. In 2010, the two largest private prison companies alone took in nearly $3 billion in revenue, and their top executives each received annual compensation packages worth well over $3 million.” (CNBC) The industry reaps $5.1 billion in government contracts annually.
Furthermore, private prisons seem committed to increasing their populations while remaining picky about who gets into their exclusive digs. “Unlike the private contractors,” the analysis said, the state “is required to provide medical and mental health services to inmates regardless of the severity of their condition.” Studies comparing the costs incurred by state-run prisons to private-prisons, we see in the state of Arizona only a 3% increase in the total cost when accounting for the health costs incurred by state facilities. (NY Times)
While studies show that private prisons in Florida only covered half of the total medical expenses needed to provide adequate services to the men and women inside their prisons.
That gap can be wider. In Florida, officials found that two private prisons spent only about half as much on health care per inmate as comparable state prisons, a difference of $9 million over two years. Florida officials say that the new plan will better balance costs, and that private prisons comply with a 7-percent-savings law. But skeptics like State Senator Mike Fasano, a Republican, fear cherry-picking may be the only way they can do that.
In Arizona, minimum-security state inmates cost 2.6 percent — or $1.39 per day — more than those in private prisons, before accounting for extra costs borne by the state. But after eliminating these, state prisoners cost only three cents more per day, the analysis found.
While private prisons are not the only facilities where inmates face neglect for medical conditions, there is a dilemma of public accountability when profiting off of a person’s incarceration, only to refuse medical services, or have shoddy procedures and protocols to account for basic treatment. The dilemma is further exacerbated when the public discovers that these prisons are not required under contractual agreement to provide adequate care. Taxpayers are supporting this treatment whether they like it or not.
Part 1: The Right to Breathe
An asthma diagnosis is not typically a death sentence. But if you are convicted of a felony, it very well could be. Perhaps this is because, like the poor, we frequently blame prisoners for their situation and thereby conveniently overlook the conditions they face.
Outside of prison, when you can’t breathe or are experiencing severe pain, regardless of your insurance situation, you can at least call 911 or go to the Emergency Room. In prison, you depend on guards and other

employees to allow you to access the services you need to (no big deal), live. And for many, that required reliance has had devastating consequences.
In Texas, Micah Burrell, a prisoner at Texas Department of Criminal Justice’s (TDCJ) McConnell Unit relied on the six guards and a prison nurse who eventually came to the scene as he cried out for help when suffering an asthma attack. Instead of following policy and administering proper medical care, the team mocked Burrell, as he was doubled over, gasping for air, for over an hour. Eventually Burrell was taken to the hospital and pronounced dead. He was 24 years old and just months away from parole.
Prior to the incident, officials had violated numerous other TDCJ policies regarding the treatment of asthma inmates. They had also denied Burrell inhalers that he needed to survive multiple times, and housed him in an individual unit, even though prisoners with asthma were not to be housed alone.
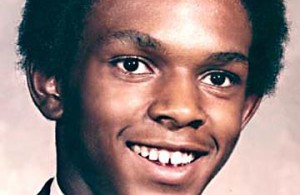
Timothy Cole, another inmate in Texas, also died in prison from a lack of adequate medical treatment for his asthma. Cole, a 39-year-old Army Veteran, passed away near the end of a 25-year sentence for a crime he did not commit. Shortly after his death, confessions of the actual perpetrator reached the Innocence Project of Texas and Cole’s family. Cole was posthumously exonerated in 2009, and pardoned in 2010. Unfortunately, the prison health care system had already killed him.
A quick Internet search reveals hundreds of avoidable prisoner deaths; cases where family members have pursued justice when loved ones died from the negligence and abuse from correctional employees.
Prevalence rates for many chronic and infectious diseases are much higher among the prison population than the general population. Varying factors contribute to these higher rates, but the frequently disadvantaged socio-economic backgrounds of inmates is certainly a strong one. With regards to asthma in particular, studies have shown that inmates in state jails are 31% more likely to suffer from the condition than non-incarcerated citizens.
“To start, prisons and jails are often poorly ventilated, dilapidated, and overcrowded–sites for transmission or exacerbation of respiratory diseases [8,9]. They offer limited exercise, or chronic disease education and self-management skills [10,11]. Moreover, individuals released from prison face legal barriers to employment, housing, public entitlements, and educational opportunities,[12-14] which may exacerbate already limited access to community health care and medical treatment.( Incarceration as a key variable in racial disparities of asthma prevalencehttp://www.biomedcentral.com/1471-2458/10/290/)
In other words, prisoners are more likely to be sick than the general public, and we ensure they leave no better off.
While only approximately 2 out of 100,000 die each year from asthma in the general population, prisoners face the real possibility of a death sentence from the illness. Concrete national data can be difficult to find because it relies upon prisons themselves to self report, and any required forms demand very limited information. As such, reporting systems don’t typically account for negligence or preventable deaths.
However, California, one of the few states to do detailed reporting regarding their healthcare system, found that asthma was the leading cause of preventable death within their prison population in 2006.
Even though compared to non-incarcerated citizens, inmates are much more likely to have asthma (as well as multiple other illnesses and infections), many prisons lack basic protocols for dealing with the condition. And for those prisons that do provide a protocol for care, employees often fall far from its requirements.
Inmates are not asking for special treatment or state of the art medical care. They are asking for an inhaler, for assistance when they struggle to breathe.
Part 2: Another Front in the War on Women